Abstract
Introduction. Renal dysfunction is commonly observed in patients with primary myelofibrosis (PMF), but its etiology remains largely unknown. Recent evidence suggests that in many cases it may be a direct consequence of PMF, rather than simply reflecting individual aging. Glomerulopathy, in fact, can be observed in PMF, presenting with mesangial proliferation and hypercellularity, likely as a consequence of abnormal cytokine expression, and case reports show that the use of ruxolitinib may improve its outcome.
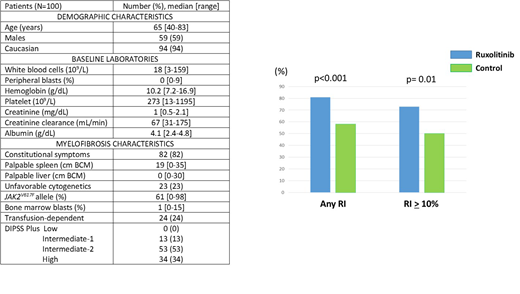
Methods. We performed a retrospective analysis of 100 patients with previously untreated PMF, receiving frontline treatment with single agent ruxolitinib at our institution between 07/2004 and 11/2013. Creatinine clearance (CrCl) values were calculated by Cockcroft-Gault equation at baseline and serially during treatment. Renal improvement was defined as best percentage change in CrCl during treatment as compared to baseline value. A group of 105 patients with PMF, receiving frontline treatment with a non-ruxolitinib-based therapy on protocol during the same time range, and matched by age, sex and CrCl, was used as control.
Results. Baseline characteristics of 100 patients with previously untreated PMF receiving frontline ruxolitinib are shown in the Table. Eighty-one (81%) patients in the ruxolitinib group had an increase in CrCl while on treatment (as compared to baseline) vs 61 (58%) in the control group (p<0.001). A renal improvement (RI) ≥ 10% was achieved in 73 (73%) patients in the ruxolitinib group and 52 (50%) patients in the control group (p=0.01), after a median time of 11 and 7 months, respectively (p=0.32)(Figure). A RI ≥ 25% was achieved in a small population sample (33% and 23%, respectively).
The association between baseline patient characteristics and achievement of a RI ≥ 10% was evaluated among all patients. On univariate analysis (UVA), factors associated with a RI ≥ 10% were non-Caucasian race (99% vs 88%, p=0.006), elevated baseline serum creatinine (1 mg/dL vs 0.9 mg/dL, p=0.05), low baseline CrCl (66 ml/min vs 78 mL/min, p<0.001) and use of a JAKi (58% vs 34%, p=0.001). On multivariate analysis (MVA), use of a JAKi maintained its independent association with a RI ≥ 10% (odd ratio 3, 95% confidence interval [CI] 1.6-5.5, p <0.001).
After a median follow-up of 41 months (range, 1-159 months), all patients failed frontline treatment, and median failure-free survival (FFS) was 14 months (range, 1-117 months). Factors associated with prolonged FFS on UVA were intermediate-1 DIPSS plus score as compared to intermediate-2 and high score (53 months vs 24 months and 6 months, p<0.001), use of ruxolitinib (39 months vs 6 months, p<0.001) and achievement of a RI ≥ 10% (24 months vs 8 months, p=0.01). Achievement of a RI ≥ 10% maintained its independent association with prolonged FFS on MVA (hazard ratio 1.4, 95% CI 1.1-2, p=0.02).
Discussion
This is the first study showing that the use of ruxolitinib is associated with improved renal function in patients with PMF. Similarly to what is done in other hematological malignancies, routine kidney biopsies in patients with PMF and unexplained renal dysfunction may shed light on its etiology and help assess the efficacy on ruxolitinib for the treatment of PMF-related glomerulopathy.
Verstovsek:Incyte: Consultancy; Italfarmaco: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal